Advancements in Non-alcoholic Fatty Liver Disease (NAFLD) Research – By Dr Harold Gunatillake
Non-Alcoholic Fatty Liver Disease (NAFLD) impacts
approximately 25% of the global population, rendering it a substantial public health issue. Initiatives aimed at enhancing screening and early detection are of paramount importance, particularly in areas with elevated rates of obesity and diabetes.
Exploring the Latest Discoveries and Treatments
Nonalcoholic fatty liver disease (NAFLD) has emerged as one of the most prevalent chronic liver conditions globally, affecting millions of individuals. Its increasing prevalence is closely
correlated with the rising rates of obesity, type 2 diabetes, and metabolic syndrome. As researchers persist in elucidating the complexities of this disease, significant advancements have been achieved in comprehending its pathophysiology, diagnostic methodologies, and therapeutic strategies.
About 100 million people (about 25%) in the United States are estimated to have Non-alcoholic Fatty Liver Disease (now called NAFLD).
The incidence of NAFLD is high among Sri Lankans. Available evidence suggests that NAFLD is the most common chronic liver disease in the country. In an extensive hospital-based study carried out recently, cryptogenic cirrhosis and alcoholic liver disease were found to be the two predominant etiological factors for cirrhosis in Sri Lanka.
Understanding NAFLD
What is NAFLD?
Liver cells have a normal amount of fat deposits stored as triglycerides. This condition, known as fatty liver disease or hepatic steatosis, occurs when excess fat builds up in the liver. While a small amount of fat is typical in the liver, excessive accumulation can lead to various complications, including inflammation (steatohepatitis) and potentially cirrhosis.
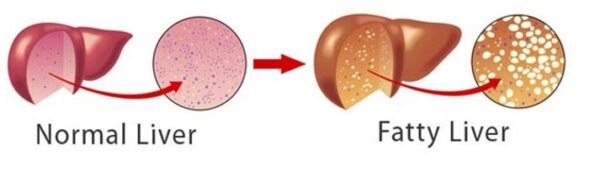
NAFLD is characterised by excessive fat accumulation in the liver, unrelated to alcohol consumption. It ranges from simple hepatic steatosis (fat buildup) to nonalcoholic steatohepatitis (NASH), which involves inflammation and liver cell damage. If left untreated, NASH can progress to fibrosis, cirrhosis, or even hepatocellular carcinoma.
Risk Factors
The primary risk factors for NAFLD include obesity, insulin resistance, type 2 diabetes, high cholesterol, and hypertension. Genetic predispositions also play a role, with specific gene variants such as PNPLA3 and TM6SF2 linked to increased susceptibility.
Obesity is a rampant issue among Sri Lankans, commonly characterised by the presence of ‘potbellies,’ in which adipose tissue is predominantly concentrated within the abdominal cavity surrounding several vital organs; this type of fat is commonly referred to as visceral fat.
Although it is not accurate to assert that nearly all individuals with uncontrolled diabetes develop non-alcoholic fatty liver disease (NAFLD), the incidence of NAFLD among those with type 2 diabetes (T2D) is notably elevated, with estimates ranging from 55% to 70%. This indicates that a considerable majority of individuals diagnosed with T2D are likely to develop NAFLD, particularly those who are also classified as overweight or obese.
Recent Developments in Diagnosis
Enhanced Imaging Techniques
Traditional methods of diagnosing NAFLD include ultrasound and liver biopsy. However, newer imaging technologies have gained prominence, such as transient elastography (FibroScan) and magnetic resonance imaging-proton density fat fraction (MRI- PDFF). These methods provide non-invasive and accurate assessments of liver fat content and fibrosis.
Biomarker Discovery
Recent research has focused on the identification of biomarkers for NAFLD and NASH. Biomarkers such as cytokeratin-18 (CK-18) and adiponectin levels are showing promise for assessing disease severity without the need for invasive procedures.
In individuals diagnosed with obesity and non-alcoholic steatohepatitis (NASH), heightened plasma CK-18 levels (exceeding 150 U/L) correlate with diminished adiponectin levels, thereby suggesting a connection between hepatic cellular damage and decreased adiponectin, a hormone pivotal for metabolic well-being. This correlation may signify a metabolic phenotype associated with obesity, wherein elevated CK-18 levels denote mild hepatic injury and metabolic complications.
Liver function tests, specifically blood tests assessing liver enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are frequently utilised to assist in the diagnosis of non-alcoholic fatty liver disease (NAFLD). Increased concentrations of these enzymes may signify liver inflammation or damage, indicating the potential presence of NAFLD.
Liver function tests are blood tests that help find the cause of your symptoms and monitor liver disease or damage. The tests measure the levels of certain enzymes and proteins in your blood as mentioned above..
Some of these tests measure how well the liver performs its regular functions of producing protein and clearing bilirubin, a blood waste product. Other liver function tests measure enzymes that liver cells release in response to damage or disease.
Irregular liver function test results don’t always mean liver disease. A health care team member will typically explain your results and what they mean.
Nevertheless, liver function tests are not always definitive and are typically employed with imaging examinations, such as ultrasound or magnetic resonance imaging (MRI), to corroborate the diagnosis.
Magnetic resonance elastography combines MRI imaging with sound waves to create a visual map, or elastogram, showing the stiffness of body tissues.

Advancements in Treatment
Pharmacological Innovations
Currently, several pharmacological agents are undergoing clinical trials aimed at addressing various aspects of the pathogenesis associated with non-alcoholic fatty liver disease (NAFLD):
** Elafibranor **: This compound functions as a dual agonist of peroxisome proliferator-activated receptors (PPAR), demonstrating efficacy in enhancing hepatic health by mitigating inflammation and fibrosis.
** Obeticholic Acid (OCA) **: As a farnesoid X receptor (FXR) agonist, OCA regulates bile acid synthesis and reduces hepatic fat accumulation.
** Semaglutide **: Initially utilised as a treatment for type 2 diabetes, semaglutide has shown promising potential in reducing liver fat and enhancing metabolic parameters.
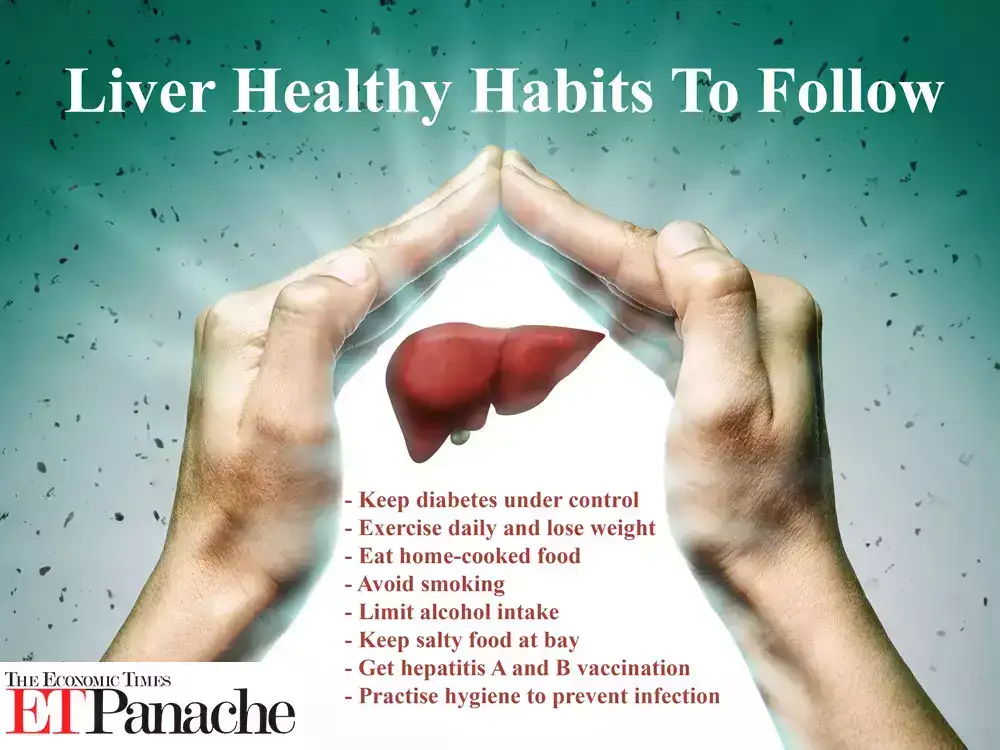
Lifestyle Interventions
While pharmacological treatments continue to evolve, lifestyle modifications persist as the cornerstone of managing Non- Alcoholic Fatty Liver Disease (NAFLD). Weight reduction achieved through dietary changes, enhanced physical activity, and behavioural interventions has been demonstrated to improve liver function and decrease fat accumulation significantly.
Gut Microbiome Research
Recent studies underscore the significance of the gut microbiome in the progression of Non-Alcoholic Fatty Liver Disease (NAFLD).
Modulating the microbiome through probiotics, prebiotics, or faecal microbiota transplantation (FMT) is currently being investigated as a promising therapeutic approach.
Therapeutic effects of polysaccharides on NAFLD
First, polysaccharides need to be defined.
Polysaccharides are a significant class of biomolecules. They are long chains of carbohydrate molecules composed of several smaller monosaccharides. These complex biomacromolecules are an essential energy source in animal cells and a structural component of plant cells.
Polysaccharides, acting as prebiotics, can potentially help manage non-alcoholic fatty liver disease (NAFLD) by modulating the gut-liver axis. They do this by influencing gut microbiota composition and function, improving intestinal barrier integrity, and reducing the translocation of harmful substances like lipopolysaccharide (LPS). This helps to reduce inflammation and improve lipid metabolism in the liver.
Modulating Gut Microbiota:
Polysaccharides can alter the composition and diversity of gut bacteria, potentially restoring a healthier balance.
They can increase the abundance of beneficial bacteria that produce short-chain fatty acids (SCFAS) essential for energy and signalling.
Polysaccharides regulate the gut microbiota and can influence the production of various metabolites, including LPS and bile acids (BAS), which can directly impact liver health.
- Improving Intestinal Barrier Function:
Polysaccharides can strengthen the intestinal barrier, reducing the permeability of harmful substances like LPS into the bloodstream.
This helps to prevent liver inflammation, which is a key factor in the development and progression of NAFLD.
A polysaccharide from jackfruit pulp has been found to improve liver function in a high-fat diet.
Global Implications and Future Directions
Personalised Medicine
Integrating genetic, metabolic, and microbiome data facilitates the advancement of personalised medicine strategies in treating Non-Alcoholic Fatty Liver Disease (NAFLD). Customised interventions derived from individual risk profiles and disease mechanisms present promising opportunities for enhanced management effectiveness.
International Collaboration
Organisations such as the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD) are spearheading collaborative initiatives to standardise diagnostic criteria, promote research, and formulate global strategies for the prevention and treatment of Non-Alcoholic Fatty Liver Disease (NAFLD).
Conclusion
Recent advancements in the research on Non-Alcoholic Fatty Liver Disease (NAFLD) underscore the intricate nature of this condition and emphasise the necessity for multidisciplinary approaches. Significant progress has been noted in the areas of imaging, biomarker discovery, pharmacological treatments, and gut microbiome modulation, so the prospects for managing NAFLD appear optimistic. Continued investment in research initiatives, awareness campaigns, and international collaboration will be crucial in addressing this escalating health concern.
This vibrant field of study persists in its evolution, offering renewed hope for the millions of individuals impacted by NAFLD and layingbthe groundwork for innovative treatments that target the underlying causes of the disease.
This topic can be a bit complicated, and you might find it helpful to read through it a few times to grasp its essence fully. I hope you find it useful, primarily as you work towards recovering from liver issues.
End
Image Source : economictimes