Myocardial Ischaemia and Infarction – By Dr. Gnana Sankaralingam
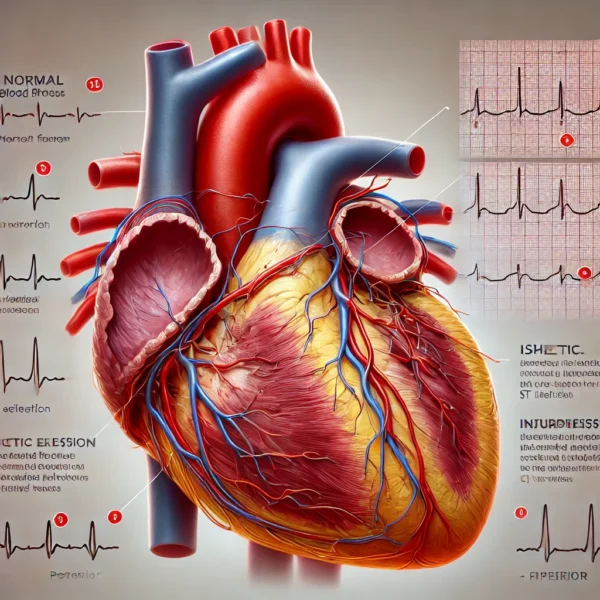
 Heart muscle must receive sufficient blood supply through its own network of arteries, called coronary arteries. Those that supply heart muscle with oxygenated blood are the left and right coronary arteries. Left coronary has two major branches, circumflex which travels to the upper lateral wall of the ventricle and the anterior descending which tracks to the anterior portion of the heart. Right coronary curves around right ventricle and separates into a variable number of branches. Base of the left ventricle is supplied by both. Narrowing of coronary artery often caused by atherosclerosis, results in diminished blood supply to the heart. During rest these narrowed coronary arteries may deliver sufficient blood supply, but with exertion the rapidly pumping thick left ventricle will require a greater blood supply, and will be the chamber to suffer by reduction in blood flow. Lack of adequate oxygenated blood results in ischaemia. If the heart is without blood supply, injury to heart muscle would occur. If blood supply does not return, death of that part will occur, termed infarction.
Heart muscle must receive sufficient blood supply through its own network of arteries, called coronary arteries. Those that supply heart muscle with oxygenated blood are the left and right coronary arteries. Left coronary has two major branches, circumflex which travels to the upper lateral wall of the ventricle and the anterior descending which tracks to the anterior portion of the heart. Right coronary curves around right ventricle and separates into a variable number of branches. Base of the left ventricle is supplied by both. Narrowing of coronary artery often caused by atherosclerosis, results in diminished blood supply to the heart. During rest these narrowed coronary arteries may deliver sufficient blood supply, but with exertion the rapidly pumping thick left ventricle will require a greater blood supply, and will be the chamber to suffer by reduction in blood flow. Lack of adequate oxygenated blood results in ischaemia. If the heart is without blood supply, injury to heart muscle would occur. If blood supply does not return, death of that part will occur, termed infarction.
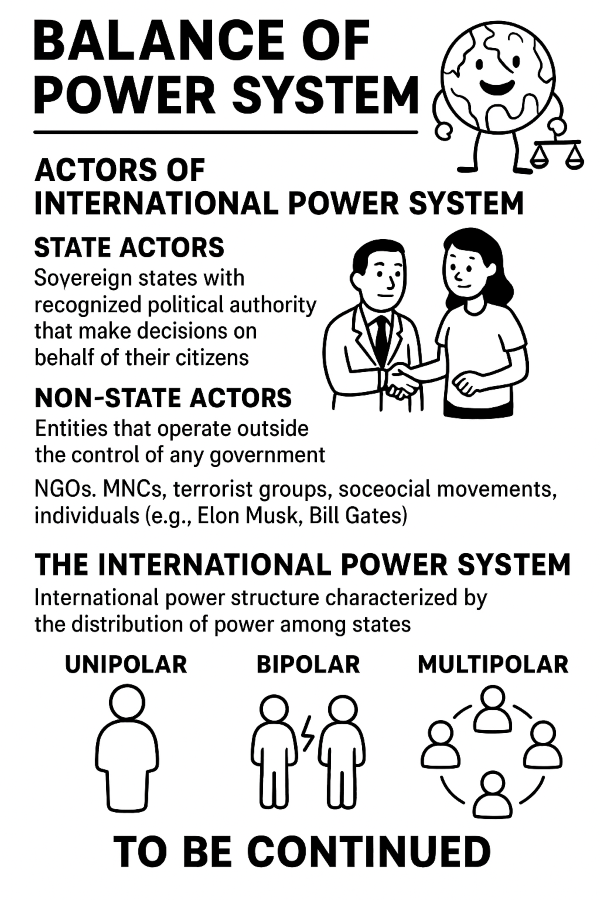
Ischaemia is lack of blood to the left ventricle and is manifested in the ECG by ST depression or symmetrically inverted T waves. All ECG leads must be checked for T wave inversion and ST depression. T inversion is normal in AVR and a normal variant in lead 3 and V1. Injury is a stage beyond ischaemia and is manifested in the ECG by ST elevation. Injury is a reversible process like ischaemia, and no permanent damage necessarily occurs. All leads in ECG should be checked for ST elevation. Infarction is necrosis or death of tissue in a part of myocardial wall and is demonstrated in the ECG by significant Q waves, which should be either 0.4 sec (one small square) wide or one third the height of R wave. If neither of these conditions is met, Q waves are not diagnostic of infarction. Septal Q waves which are found normally in Leads 1, AVL, V5 and V6 represent depolarisation of ventricular septum and are not pathologic. In infarction, electrical forces from damaged left ventricles are nonexistent, so that electrical forces from right ventricles are unopposed to produce a deep and wide Q wave as they move away from the electrode during activation of infarcted area.
The diagnosis of myocadial infarction depends on history and examination and on measurement of biochemical markers of cardiac muscule damage and ECG. Rise in level of Troponin I or T in patients with suggestive history is taken to mean that MI has occurred but treatment still depends on ECG. The term “Acute Coronary Syndrome” is used to include MI with ST segment elevation on ECG, MI with Treponin rise but either T wave inversion or ST segment depression, chest pain with ST segment depression but no treponin rise (used to be called unstable angina) and sudden deaths due to coronary disease. Term stable angina is a diagnostic label given to those with chest pain for whom above is inappropriate. Sequence of features characteristic of an ST segment elevation or full thickness MI are: initially normal ECG, followed by elevation of ST segment over injured area, development of Q waves over infarcted area, T wave invertion over infarcted area with ST elevation remaining, return of ST segment to baseline with T invertion remaining. The ECG leads that show changes typical of a myocardial infarction depend on which part of the heart that was affected.
Determine approximately which area is affected. Left ventricle is divided into four main locations as anterior, lateral, inferior and posterior. Leads V1, V2, V3 and V4 are positioned over anterior part, leads 1, AVL, V5 and V6 are positioned over lateral part and leads 2, 3 and AVF are positioned over inferior part of left ventricle. No leads are put directly over posterior aspect, but by observing changes in opposite or anterior wall, some inference can be made. Electrically the infarcted muscle can be classified into three regions: infarcted region where heart muscle is electrically dead and does not conduct any impulses, injured region which immediately surrounds infarcted area and has cell membranes that are never completely polarised and ischaemic region where repolarisation is impaired.
Infarction can be determined by identifying significant Q waves in at least two ECG leads in each infarct location or by noting loss of R wave potential. In anterior infarcts, Q wave will be found in leads V1, V2, V3 or V4. In antero-septal infarcts, Q waves will be in V1 and V2 only or poor R wave progression in V1 and V2, which could also be caused by left ventricular hypertrophy. In lateral infarcts, Q waves will be in leads 1, AVL and V5 or V6 and in inferior infarcts, Q waves will be in leads 2, 3 or AVF. In posterior infarcts, there would be tall R waves, often accompanied by tall T waves in the anterior leads, and also depressed ST segment. Suspect posterior infarct if tall R waves are in V1 and V2 in the presence of inferior infarct. Infarctions could occur either as isolated or in various combinations such as anterior and lateral, as anterior, lateral and inferior or as inferior, posterior and lateral.
Inferior infarction is sometimes associated with infarction of right ventricle. It is suspected clinically, when the lungs are clear but the jugular venous pressure is elevated in a patient with inferior infarction. In ECG leads recorded from right side of the heart such as V1R, V2R and V3R, corresponding to left side leads of V!, V2 and V3 respectively, there will be ST segment elevation. In posterior infarction, the rearward moving electrical forces are lost, thus V1 sees the unopposed forward moving depolarisation of right ventricle and records predominantly upright QRS complex. If chest electrodes are moved from left axilla on to back to V7 to V12 positions, raised ST segments and Q waves typical of acute infarcts will be seen. When infarction does not involve the whole thickness of the ventricular wall, no electrical window will be formed and so there will be no Q waves (non-Q wave infarct) also called “sub-endocardial infarction”. However there will be abnormality of polarization that leads to T wave inversion. Non ST elevation infarction (NSTEMI) is usually due to partial blockage in a branch off main coronary artery. NSTEMI extends to portions of the wall only unlike ST elevation MI which causes transmural damage. In both non-Q wave infarction and NSTEMIs, Troponin level is very high compared to the ST elevation infarctions.
Treatment of acute coronary syndrome (ACS) vary depending on ECG changes and Troponin level. In unstable angina where there is ST depression and no rise in Troponin level and in NSTEMI where there is ST depression and rise in Troponin level, management is pain relief, thinning of blood with aspirin and low molecular wieght heparin, while in STEMI in addition to above, angiography and stenting of blocked arteries performed.